PROVIDENCE, R.I. [Brown University] — With findings from four recent reports by the Government Accountability Office, the new Congress could close dozens of loopholes that have allowed physicians to increasingly refer patients for medical services to enterprises in which they have a financial stake, write the authors of a new “Viewpoint” in JAMA. Ending the controversial practice might save the federal government hundreds of millions of dollars a year.
The practice of “self-referral” has a logic, acknowledged article co-author Dr. Eli Y. Adashi, professor of medical science in the Alpert Medical School and former dean of medicine and biological sciences at Brown University. A doctor may have good reason to tell a wheezing smoker that he needs a CT scan of his lungs. If that doctor happens to own diagnostic imaging clinic in the same building, the logistical convenience for the patient and the rapid and seamless reporting of the results back to the doctor may be hard to beat. But is the CT scan truly necessary? Is that CT machine really the best one available to the patient at comparable cost? Will it be read by a radiologist or by a less well-trained technician? Given the financial ties involved, is the doctor’s focus solely on providing the best care, or is it blurred by the chance to claim a greater share of the patient’s – and Medicare’s – money?
“It is capitalism at its best and at its worst,” Adashi said. “It’s important to point out the uncomfortable relationship between money and medicine.”
Policymakers have wrestled with the issue for decades. In 1989 and 1993, Congress passed two laws, nicknamed “Stark I” and “Stark II,” that ostensibly prohibited physician self-referrals. But 35 exceptions have allowed the practice to thrive instead, wrote Adashi and co-author Dr. Robert Kocher, a senior fellow at the University of Southern California.
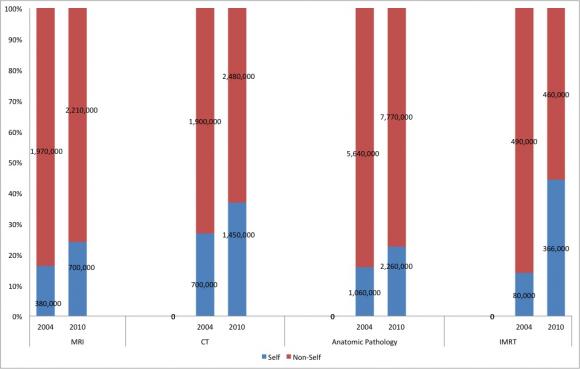
The GAO’s series of reports, which concluded in June, found that for three different services — MRI and CT scans, anatomic pathology, and intensity-modulated radiation therapy — self-referrals gained substantial market share at the expense of non-self-referrals between 2004 and 2010.
“Observations on self-referrals of IMRT services for the treatment of prostate cancer were particularly disconcerting,” Adashi and Kocher wrote. “The utilization of self-referred IMRT services increased by as much as 356 percent at a time when the utilization of the non-self-referred variety decreased by 5 percent.”
In the long term, the authors note, self-referrals may decrease as health care payment models change from the current “fee-for-service” model to an alternative — such as accountable care organizations, in which doctors are rewarded for achieving quality outcomes in as cost-effective manner as possible. But that model shift will take years and might never happen completely.