PROVIDENCE, R.I. [Brown University] — Home-delivered meals bring not only food to seniors but also the opportunity to remain in their homes. A new study by Brown University public health researchers projects that if every U.S. state in the lower 48 expanded the number of seniors receiving meals by just 1 percent, 1,722 more Medicaid recipients avoid living in a nursing home and most states would experience a net annual savings from implementing the expansion.
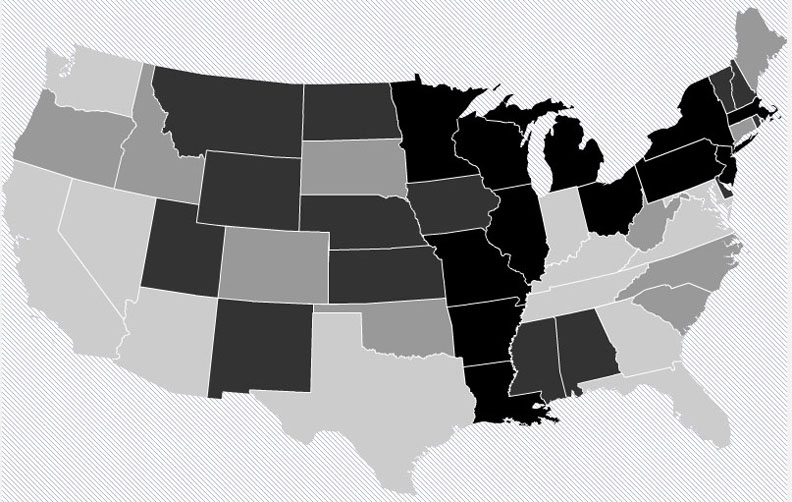
Pennsylvania would see the greatest net savings – $5.7 million – as Medicaid costs for nursing home care dropped more than costs rose for delivering the additional meals. But every state is different. Florida would see a net cost of nearly $11.5 million instead. Overall, 26 states would see a net savings according to the analysis published in the October issue of the journal Health Affairs, while 22 would end up spending more.
Every state would enable more seniors, who could live independently except for meals, to remain in their homes regardless of whether they are on Medicaid.
Study lead author Kali Thomas, assistant professor (research) in the Brown University School of Public Health, said the study provides guidance for state policymakers as they the consider the future of their home-delivered meals programs, which are conducted under the Older Americans Act.
“We wanted to provide a roadmap for people,” Thomas said.
State by state
To do the study, Thomas and co-author Vincent Mor, the Florence Pirce Grant Professor of Community Health, looked at several key pieces of data, including how many seniors in each state receive home-delivered meals and how much it costs each state to provide those meals. She and Mor also looked at nursing home and Medicaid data to estimate the number of seniors that Medicaid maintains in nursing homes who are “low-care,” meaning they may have the functional capabilities to live at home. Finally they looked at the per diem Medicaid pays in each state for seniors to live in nursing homes.
The results allowed them to estimate the incremental cost of providing meals to 1 percent more seniors in each state, the number of additional seniors on Medicaid who would no longer need to live in nursing homes, and how much less Medicaid would therefore spend in each state.
Across the country, the 1 percent expansion would bring meals to 392,594 more seniors at a cost of more than $117 million. Because 1,722 seniors would no longer have to live in nursing homes on Medicaid, total Medicaid savings would total $109 million.
The reason why the additional food delivery costs outstrip Medicaid savings nationwide, even though most states would save money on a net basis, is that in some very large states with relatively few low-care seniors or relatively low Medicaid per diems, food costs outweighed the resulting Medicaid savings on a relatively large scale.
“In states like California and Florida where a 1-percent increase in the 65-plus population is a lot of people, it will cost those states a lot more to feed them,” Thomas said.
But, as she and Mor wrote in Health Affairs, “Our analyses suggest that 26 states with high Medicaid nursing home per diem reimbursement rates, a large proportion of low-care [nursing home residents on Medicaid], and a relatively small population of older adults, could save money.”
Thomas said states projected to lose money can opt to focus their efforts in ways that are more precise than an across-the-board expansion.
“We’re not proposing that all states simply increase the proportion of age 65 plus receiving meals by 1 percent,” she said. “But if they were to target these vulnerable people who are at risk for nursing home placement they would likely see more savings. This is a program that has the potential to save states a lot of money if it’s done correctly.”
More than money
Policymakers should consider not only the fiscal implications of providing home-delivered meals, which the study quantifies, but also the impact on individual seniors, said Thomas, who has seen the benefits anecdotally as a Meals on Wheels volunteer in Rhode Island.
“The quality of life argument is really important, but it’s not been shown, empirically,” Thomas said.
That will soon change. With a $350,000 grant from the American Association for Retired Persons Foundation and Meals on Wheels, Thomas is beginning a randomized controlled trial made possible by the fact that, especially amid the federal budget sequester, there is a waiting list among seniors to receive meals.
In the study 200 seniors will receive meals daily, 200 more will receive a delivery of frozen meals once a week and then another 200 will continue on the waiting list as before as a control group. The study will compare quality of life, isolation, and health care utilization among individuals before and after they begin receiving meals and across the three groups.
The results will provide evidence to researchers and policymakers of the impact of home-delivered meals. Seniors, of course, already know what it means to them.
The National Institute on Aging (grant P01 AG-027296) and the Agency for Healthcare Research and Quality (T32, HS-000011) funded the research.

