PROVIDENCE, R.I. [Brown University] — A new study of the relationship between violent conflict and HIV incidence in sub-Saharan Africa finds that HIV incidence may be at its worst in the period before hostilities break out. The Brown University analysis reports that the rate of new infections rises significantly in the five years leading up to bloodshed.
“It implies that there is something going on in social, political, and health care environments in those years that are conducive to HIV spread,” said Brady Bennett, lead author of the study published in the journal PLOS ONE.
Prior studies examining how war may affect the HIV epidemic have produced mixed, and even conflicting, results, said senior author Mark Lurie, associate professor of epidemiology in the Brown University School of Public Health. Lurie and Bennett, who was earning a Master of Public Health degree at Brown, worked together to produce a more comprehensive data set than had existed before and to conduct more rigorous analysis than had previously been done.
The new study tracked HIV incidence statistics in 36 sub-Saharan countries from 1990 through 2012 and correlated them with periods of conflict and peace in each country. The research team was therefore able to calculate how the incidence rose and fell in each country in relation to violence, while controlling for other factors such as economic development, refugee influx, and the year of the region’s broader epidemic, which generally peaked in 1996.
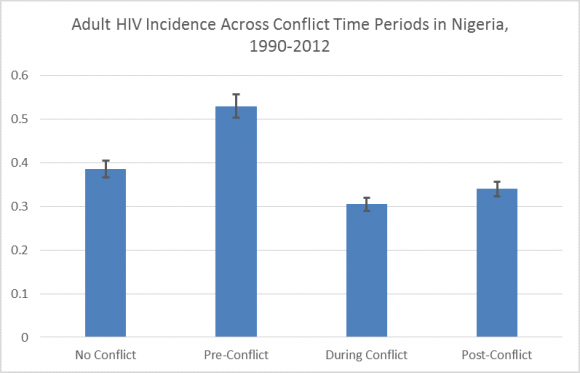
Compared to times of peace, the analysis showed, HIV incidence increased by 2.1 infections per 1000 people a year in the five years before a conflict where at least 25 people died as a result of fighting. The researchers also found that during conflict the incidence rate declined by 0.07 infections per 1000 people, compared to times of peace. The study defines conflict as violence that claims at least 25 battle-related deaths. Researchers found that as conflicts became more bloody, HIV incidence tended to drift down a bit more.
Each country had a different HIV trajectory through war and peace (some had no conflict at all), but countries such as Burundi, Eritrea, Nigeria, and Uganda all endured their highest HIV incidence rates in periods before conflict and lower rates during conflict.
The study does not explain what is going on overall or in any single country that might account for changes in HIV incidence. Bennett said the finding that HIV incidence might decline during intense conflict is likely not because conflict somehow makes anything better. Instead, he said, fighting likely undermines accurate data collection, leaving many new infections undetected.
But he said research is urgently needed, in light of the findings, to understand how the descent into conflict may lead to faster HIV spread. Determining the answers could make governments and aid organizations more effective in preventing the problem from arising.
The findings suggest that waiting to intervene until conflict is already underway may miss a major opportunity to prevent new infections.
“What our paper points to is that we need to better understand the precipitating factors that drive conflict precisely because we’ve identified that as a period of particular vulnerability where HIV incidence is likely to be increased,” Lurie said.
In addition to Bennett and Lurie, the paper’s other authors are Brown University public health faculty members Brandon Marshall, Annie Gjelsvik, and Stephen McGarvey.