PROVIDENCE, R.I. [Brown University] — The revolution that optogenetics technology has brought to biology — neuroscience in particular — could be transformed all over again if a new project getting underway at Brown University and Central Michigan University (CMU) is successful.
First introduced in a practical form in 2005, optogenetics gave brain scientists the amazing new capability to use pulses of laser light to control almost any type of neuron in any area with precise timing. Prior means of controlling neurons weren’t ideal. Electrical pulses were powerful but drove all the cells in an area, not just desired cell types. Drugs couldn’t confine control to a particular area and didn’t have precise timing. Optogenetics could do it all by genetically engineering cells to become excited or suppressed by different colors of light.
But optogenetics can still do more, said Christopher Moore, associate professor of neuroscience at Brown, who leads the new project, funded by a new $1-million grant from the W.M. Keck Foundation. His goal is to make cells “smart” enough to emit light precisely when needed in order to optogenetically control themselves or their neighbors. If optogenetics is ever approved for human use, this new form of self-regulation — which would not involve injecting light into the body from outside — could produce new ways to treat problems ranging from epileptic seizures to Parkinson’s disease to diabetes.
‘BL-OG,’ and beyond
In 2013, Moore’s collaborator Ute Hochgeschwender, associate professor at CMU, demonstrated how to make optogenetic cells emit their own light using a capability widely found in nature: bioluminescence. Bioluminescence is the natural chemical reaction that allows fireflies and many sea creatures to make light. The advance of pairing bioluminescence with optogenetics allowed scientists to make the technology wireless. In most optogenetic experiments, laser light is delivered into the body by a fiber optic cable, but with BL-OG — shorthand for BioLuminescent-OptoGenetics — a cool, biologically compatible light could be triggered in cells just by administering a drug.

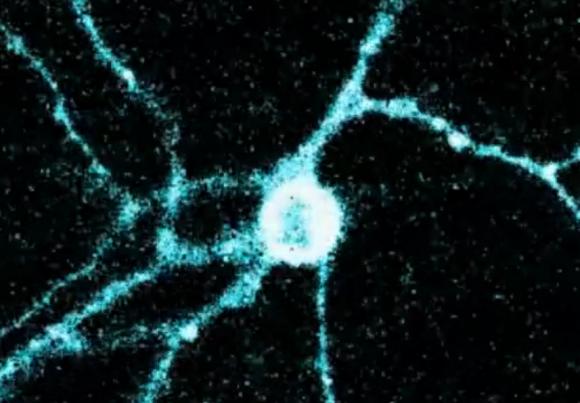
In most optogenetics experiments, light is delivered to cells from lasers through fiber optic cables. A new research project focuses on making cells produce their own light, letting them control their own activity or the activity of neighboring cells. Photo: Mike Cohea/Brown University
Now the team of Moore, Hochgeschwender, and Brown professors Barry Connors, Julie Kauer and Diane Lipscombe, interim director of the Brown Institute for Brain Science, will pursue the next big step.
“In the new grant, what we’re doing is taking BL-OG and bringing it to where it starts to get transformatively different from anything else that’s existed,” Moore said.
The idea is to program BL-OG cells to emit their light when they sense a need. As living entities, cells spend their lifetimes sensing their environment and carrying out genetic instructions to implement complex activities, such as expressing proteins, generating energy, or even countering threats. Why not try to combine that programmability with BL-OG to help cells help each other or themselves?
“Right now I could give a pill that makes cells glow and it would have an effect for a period of time,” Moore said. “What would be really neat is if we could regulate a circuit only when it’s behaving badly. What you’d love to do is let the cell have its normal pattern of activity, and then intercede at that [problematic] moment. It’s a real-time feedback approach.”
Epilepsy, for example
The team plans to try out that idea by focusing on the flow of calcium ions among cells in various parts of the body, a particular area of Lipscombe’s expertise. Calcium excites cells, such as neurons, by building up positive charges in them until they cross a threshold for action. In epilepsy, for example, there is too much of that excitation. Connors has studied that in detail.
Here is how the team proposes to help: With BL-OG, they already know how to make target cells capable of emitting and/or responding to light. The next step is to link those capabilities to sensing the levels of calcium ions. Synthetic biology, in which scientists add snippets of DNA instructions to the genome of a cell or whole organism to essentially program in a new capability, offers one potential way to make that feasible.
In the example of epilepsy, BL-OG-enabled neurons in the brain could be programmed to glow red (like a traffic light) if calcium ions are surging in too quickly. That red glow could trigger neighboring optogenetic cells to dampen their excitation amid the calcium buildup, effectively stopping a seizure as soon as it starts.
“A similar effect could normalize brain activity in Parkinson’s disease, where runaway bursting in specific brain areas is thought to underlie the symptoms of that disorder,” Moore said.
Moreover, optogenetics works in other parts of the body. In the pancreas, the team hopes to see if it is possible to program BL-OG-capable cells to sense low blood glucose levels. Calcium ions have an important role in insulin secretion, so when sugars are too low, cells programmed to be self-regulating could trigger a glow of light to optogenetically increase the excitation of cells involved in signaling insulin production.
“In the grant we propose to explore a whole variety of different targets,” he said. Another is smooth muscle cells, which also depend on calcium and are the main regulator of blood pressure throughout the body. A wide array of problems could be aided by enhancing the quality of vascular control in the brain and in the body, Moore said.
The research, supported by matching funds from Brown and CMU, is just beginning. At the end of the project, which is supported primarily for three years, Moore said he hopes he and his colleagues will have radically extended optogenetics from a technology that allows scientists to control cells in the lab into one that enables cells to control themselves and each other.
The W.M. Keck Foundation
Based in Los Angeles, the W. M. Keck Foundation was established in 1954 by the late W.M. Keck, founder of the Superior Oil Company. The Foundation’s grant-making is focused primarily on pioneering efforts in the areas of medical, science, and engineering research. The Foundation also maintains an undergraduate education program that promotes distinctive learning and research experiences for students in the sciences and in the liberal arts, and a Southern California Grant Program that provides support for the Los Angeles community, with a special emphasis on children and youth from low-income families, special needs populations and safety-net services. For more information, please visit www. wmkeck.org.