PROVIDENCE, R.I. [Brown University] — Studies consistently show that people born weighing 6 pounds or less face an increased risk for type 2 diabetes as adults. A new study not only confirms that risk in a sample of more than 3,000 women but also shows the relative predictive value of different biomarkers, giving doctors potential new tools for understanding individual risk among low birthweight women.
The findings also could help guide researchers trying to tease out which physiological processes might be sent awry by low-birth weight, ultimately leading to type 2 diabetes.
“We are trying to understand what proportion of the risk attributable to low birthweight can indeed be explained by these biochemical intermediates, to understand the relative importance of each pathway,” said study senior author Dr. Simin Liu, professor of epidemiology and medicine at Brown University.
The research, published in the journal Diabetologia, drew on the detailed health records of participants in the Women’s Health Initiative, a huge study supported by the National Heart Lung and Blood Institute. Liu’s team focused on 1,259 women who developed type 2 diabetes and 1,790 otherwise similar women who did not.
Overall the data showed that low birthweight (less than 6 pounds) portended a 2.15 times greater risk of developing type 2 diabetes compared to women born between 8 and 10 pounds. This risk calculation adjusted for a variety of other possible confounding variables such as smoking, drinking, exercise, diet, body-mass index, race, ethnicity, and family history of diabetes. Compared to women born between 6 and 8 pounds, low birthweight women had a risk that was 1.27 times greater.
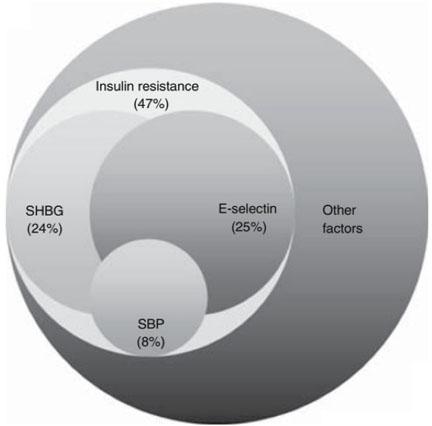
The study also looked at the relative predictive value, measured in percentages, of various readily measurable biomarkers. Among them insulin resistance contributed most strongly (accounting for 47 percent), which is not surprising because insulin resistance is a core component of diabetes. High levels of E-selectin, a marker of problems with blood vessel lining, accounted for 25 percent, low levels of sex-hormone binding globulin contributed 24 percent, and high systolic blood pressure’s mediation emerged at 8 percent from the statistical analysis.
Each of these calculations also controlled for potential confounding variables. Percentages do not add to 100 because some pathways of the risk factors may overlap.
Liu and his co-authors, including lead author Dr. Yan Song a visiting postdoctoral fellow, said they hope the findings will give doctors a refined understanding of relative risk among low birthweight women.
“These prospective data provide quantifiable mechanistic evidence linking low birthweight to increased risk of type 2 diabetes, while presenting risk stratification in a population at greater risk of developing type 2 diabetes later in life,” they conclude.
In addition to Liu and Song, the paper’s other authors are Yen-Tsung Huang, Yiqing Song, Andrea Hevener, Kelli Ryckman, Lihong Qi, Erin LeBlanc, Rasa Kazlauskaite, and Kathleen Brennan.
The National Institutes of Health (grants: R01DK066401, R21DK084482) and the Burroughs Wellcome Fund supported the study.