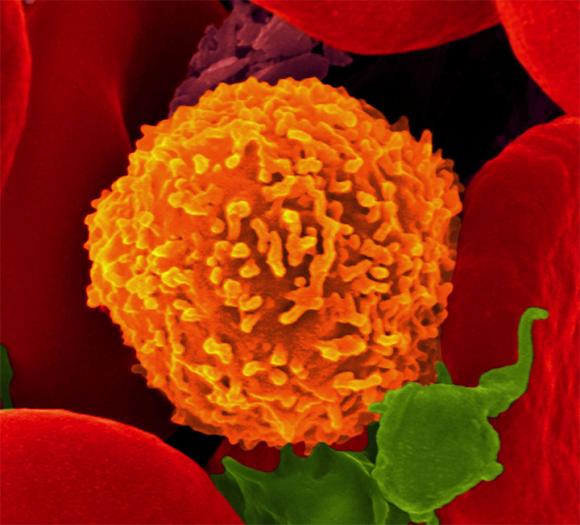
PROVIDENCE, R.I. [Brown University] — Scientists think of CD8 T cells as long-lived cells that become tuned to fight just one pathogen, but a new study finds that once CD8 T cells fight one pathogen, they also join the body’s “innate” immune system, ready to answer the calls of the cytokine signals that are set off by a wide variety of infections.
Think of CD8 T cells as soldiers who are drafted and trained for a specific mission, but who stay in service, fighting a variety of enemies throughout a long career.
CD8 T cells therefore have more utility than researchers may have realized. These findings, published in the journal mBio, suggest that the innate immune system can change with the body’s experience to have a growing number of the adaptive CD8 T cells contributing, said Christine Biron, professor of medical science at Brown University and senior author of the paper. The research may have important implications for vaccine design.
Enlightening experiments
By conducting several experiments in mouse models, Biron, lead author Jenny Suarez-Ramirez, and their co-authors tracked how CD8 T cells acquire both sensitivity for a specific virus (so-called “adaptive” immunity) and the ability to respond to more general cytokine signals of infection (“innate” immunity).
They began by picking up where a prior study had left off. They had found that upon confronting their first infection, CD8 T cells came to harbor much more of a protein called STAT4. That protein is one of the reasons that natural killer (NK) cells, the acknowledged stalwarts of innate immunity, are sensitive to cytokines.
In the new study they infected mice with the LCMV virus and then extracted CD8 T cells eight days later to observe them in culture with various cytokines, or just in plain medium as experimental controls. Some T cells had become tuned to LCMV and some had not. They found that the cells that had become tuned to LCMV were much more responsive to cytokines than cells that had not.
In another experiment to determine whether it was STAT4 that gave the T cells this cytokine responsiveness, the scientists infected mice with LCMV twice. Some of the mice in this experiment had been genetically engineered to lack STAT4 while others were normal controls. Both sets of mice developed CD8 T cells that responded to LCMV after the first infection (via their specifically tuned “antigen” receptors), but only the mice with STAT4 produced an innate response via cytokine receptors during the second infection.

“I’m saying you can take your CD8 T cells and have features of innate immunity. [CD8 T cells] give you a lot more flexibility in the kinds of activating receptors they can use.”
Then the scientists wanted to see how the CD8 T cells of LCMV-experienced mice responded to a new infection with a different virus compared to CD8 T cells of mice without LCMV experience. So they infected mice of both types with a virus called MCMV. The CD8 T cells of the mice that had already grappled with LCMV responded rapidly because of the cytokines associated with the new invader. The CD8 T cells of the “naïve” mice, meanwhile, did not produce a rapid cytokine response.
“Thus, at times of innate cytokine expression, the LCMV-specific CD8 T cells in immune mice were capable of responding to an unrelated viral infection with pSTAT4 activation,” the authors wrote. The response was evident in their expression of the important immune triggering protein IFN-gamma.
So in the face of a new invader, the veterans of LCMV exposure reacted innately.
“Because of their experience, they got conditioned to now see innate cytokines the way NK cells were seeing them at the beginning,” Biron said. “Once we’ve made these antigen-specific cells, then we have a subset of memory CD8 [CD8 T] cells that still have the specificity for an antigen, but they are also changed now so their relationship with innate cytokines looks like NK cells.”
Implications for vaccines
When developing vaccines, scientists are trying make the immune system respond as strongly as possible to a specific invader. A lot of vaccine developers are now trying to find ways to pull NK cells into that induced adaptive immune response, Biron said. But they didn’t know the opposite was already happening: adaptively inclined immune cells such as CD8 T cells were in fact also joining the innate immunity force.
“Here I’m saying you can take your CD8 T cells and have features of innate immunity,” Biron said. “The thing the T cells do is they give you a lot more flexibility in the kinds of activating receptors they can use. They can substitute for a lot of the things that NK cells can do early, that are cytokine dependent, but they also carry along with them the antigen-specificity of their receptors.”
So it may be profitable in vaccine development to try to push CD8 T cells harder. When CD8 T cells are exposed to the specific virus they are tuned for, they multiply greatly, a process called expansion.
“If you keep selecting those and expanding those you are going to make the pool of that subset higher than the pool of NK cells with time,” Biron said. “You can use them for some of the early responses that NKs do but still have the specificity dependent on their antigen receptor.”
With CD8 T cells, in other words, one gets two kinds immunity for the price of one.
In addition to Biron and Suarez-Ramirez, the paper’s other authors are Margarite Tarrio, Kwangsin Kim, and Delia Demers.
The National Institutes of Health supported the research (grant: AI05567).