PROVIDENCE, R.I. [Brown University] — A new study shows that adipose-derived human stem cells, which can become vital tissues such as bone, may be highly resistant to the common chemotherapy drug methotrexate (MTX). The preliminary finding from lab testing may prove significant because MTX causes bone tissue damage in many patients.
MTX is used to treat cancers including acute lymphoblastic leukemia, the most common form of childhood cancer. A major side effect of the therapy, however, is a loss of bone mineral density. Other bone building stem cells, such as bone marrow derived stem cells, have not withstood MTX doses well.
“Kids undergo chemotherapy at such an important time when they should be growing, but instead they are introduced to this very harsh environment where bone cells are damaged with these drugs,” said Olivia Beane, a Brown University graduate student in the Center for Biomedical Engineering and lead author of the study. “That leads to major long-term side effects including osteoporosis and bone defects. If we found a stem cell that was resistant to the chemotherapeutic agent and could promote bone growth by becoming bone itself, then maybe they wouldn’t have these issues.”
Stem cell survivors
Originally Beane was doing much more basic research. She was looking for chemicals that could help purify adipose-derived stem cells (ASCs) from mixed cell cultures to encourage their proliferation. Among other things, she she tried chemotherapy drugs, figuring that maybe the ASCs would withstand a drug that other cells could not. The idea that this could help cancer patients did not come until later.
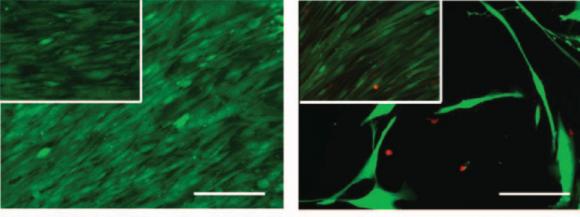
In the study published online in the journal Experimental Cell Research, Beane exposed pure human ASC cultures, “stromal vascular fraction” (SVF) tissue samples (which include several cell types including ASCs), and cultures of human fibroblast cells, to medically relevant concentrations of chemotherapy drugs for 24 hours. Then she measured how those cell populations fared over the next 10 days. She also measured the ability of MTX-exposed ASCs, both alone and in SVF, to proliferate and turn into other tissues.
Beane worked with co-authors fellow center member Eric Darling, the Manning Assistant Professor in the Department of Molecular Pharmacology, Physiology and Biotechnology, and research assistant Vera Fonseca.
They observed that three chemotherapy drugs — cytarabine, etoposide, and vincristine — decimated all three groups of cells, but in contrast to the fibroblast controls, the ASCs withstood a variety of doses of MTX exceptionally well (they resisted vincristine somewhat, too). MTX had little or no effect on ASC viability, cell division, senescence, or their ability to become bone, fat, or cartilage tissue when induced to do so.
The SVF tissue samples also withstood MTX doses well. That turns out to be significant, Darling said, because that’s the kind of tissue that would actually be clinically useful if an ASC-based therapy were ever developed for cancer patients. Hypothetically, fresh SVF could be harvested from the fat of a donor, as it was for the study, and injected into bone tissue, delivering ASCs to the site.
To understand why the ASCs resist MTX, the researchers conducted further tests. MTX shuts down DNA biosynthesis by binding the protein dihydrofolate reductase so that it is unavailable to assist in that essential task. The testing showed that ASCs ramped up dihydrofolate reductase levels upon exposure to the drug, meaning they produced enough to overcome a clinically relevant dose of MTX.
Toward a therapy?
Now that the researchers are aware of ASC’s ability to resist MTX, they are eager to see if they can make progress toward delivering a medical benefit for cancer patients. They plan several more experiments.
One is to test ASC survival and performance after 48- and 72-hour exposures to MTX. Another is to begin examining how the cells fare in mouse models of chemotherapy. They also plan to directly compare ASCs and bone marrow-derived stem cells amid various chemotherapies.
Darling said his team hopes it can make a contribution by helping patients heal from chemotherapy, which does what it must, but at a cost.
“The first step is to save a life,” he said. “Chemotherapies do a great job of killing cells and killing the cancer, and that’s what you want. But then there is a stage after that where you need to do recovery and regeneration.”
Further research will reveal whether stem cells can be part of that process.
The National Institutes of Health (grants R01AR063642, P20GM104937) and the National Science Foundation (CBET1253189) supported the research.