PROVIDENCE, R.I. [Brown University] — People with type 2 diabetes can make insulin but their bodies use it so poorly that glucose levels run amok. It’s been difficult for scientists to understand what’s going awry in the way that tiny, fast-moving proteins signal and regulate glucose metabolism. As a result, while drugs can help somewhat, many patients still must monitor their glucose and inject insulin.
Brown University biochemist Wolfgang Peti is new to the fight, but he’s well-armed and well-motivated to join it.
As it is for millions of people around the world, the pervasive condition is personal for Peti. His grandmother battled it for decades.
“It affected her ability to see, her ability to walk through the mountains of Austria, and her ability to eat all the traditional foods she grew up eating and cooking,” Peti said. “And while she successfully battled the disease for many years, eventually the doctors had to amputate both of her legs (first at age 80, second at age 88) and she was confined to a wheelchair for the last eight years of her life.”
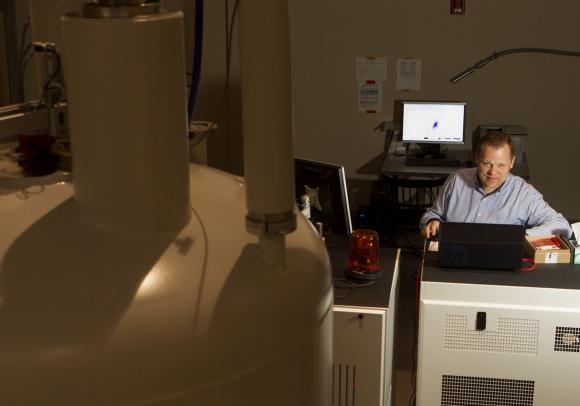
Although he hasn’t focused specifically on diabetes before, decades of research have given him a deep expertise in the atomic structure and behavior of some of the key proteins of insulin signaling. He and his collaborators have refined these proteins in the lab to the degree that they and their interactions can now be fully analyzed with advanced techniques such as nuclear magnetic resonance spectroscopy and X-ray crystallography.
Last year, when Brown acquired a powerful new NMR magnet, Peti gained a rare degree of capability to study the dynamic motions of these proteins and the timing of their interactions, as well as their basic structure. That’s exactly what he now plans to do with a five-year, $1.625-million New to Diabetes Research Accelerator Award announced Jan. 9, 2014, by the American Diabetes Association. Peti is one of only five researchers around the country to win an ADA Accelerator Award this year.
Peti’s ambitious goal is to enable the development of medicines that improve on the status quo so greatly that insulin injections might no longer necessary.
“The easiest thing would be if you have type 2 diabetes instead of injecting insulin, you’d just take a tablet,” he said. “If you can control the insulin-signaling pathway with a drug, that would make your life much easier.”
Three targets
Many brilliant scientists share this goal, but so far the field has fallen short. Still, for all the well-worn dead ends, Peti still sees the insulin-signaling pathway as rife with potential new leads. He plans to look in novel ways and in novel places at the interactions of three main proteins in particular.
One target is the binding between insulin and the insulin receptor. That step activates the “TK” domain, or section, of the receptor, kicking off the cascade of protein signaling that leads to the metabolism of glucose. This may seem like an obvious place to start, but the complexity comes from trying to observe the movements of the TK domain and the specific timing that may be going awry in type 2 diabetes.
Peti and his colleagues have been able to model it all in E. coli bacteria, which will allow them to observe it precisely with NMR. That will allow Peti see how the TK domain reshapes and moves, how quickly and when. That could yield a clear understanding of whether a drug could block or slow a key movement that is happening too soon or too quickly.
Peti also plans to work with fellow Brown biologist Marc Tatar to take the ideas into the fruit fly where they can investigate the differences made by known genetic mutations.
Another target is an enzyme called PTP1B, which can shut off insulin signaling. Because the goal in treating type 2 diabetes is to improve insulin function, Peti wants to stop PTP1B.
PTP1B has proven time and again to be tough to block without unintended consequences, but Peti hopes a less direct approach than others have taken will make a difference. Rather than targeting the main catalytic parts of the enzyme directly, he’s looking at the behavior of a more peripheral but nevertheless influential structure called the “c-terminal segment.” It’s an underexplored region that could be targeted very specifically, likely with a combination of surgical strikes on more than one area. A key requirement of any drug is that it only affects insulin signaling and not other interactions by similar enzymes.
Sure enough, along with colleague Nicholas Tonks at the Cold Spring Harbor Laboratory, Peti has begun to characterize a drug that works in this area. They plan to use NMR to improve the understanding of the drug’s workings further and use that knowledge to improve its abilities.
Peti’s third approach under the ADA award is more traditional in that it depends “simply” on characterizing the structure of a complex of proteins, together known as GM:PP1. That complex controls the balance between storing glucose in the form of a larger “glycogen” molecule and breaking glycogen down into glucose. GM:PP1 accomplishes the latter by turning on an enzyme called glycogen phosphorylase.
Peti’s idea is to figure out how a drug could inhibit GM:PP1’s recognition of glycogen phosphorylase so that it doesn’t break down glycogen into glucose so readily. Peti already knows where he wants to look on the proteins to try the idea and has developed a means of screening drugs that might interact with those areas.
Success with any of the three approaches is hardly guaranteed, but if there is a chance he can save anyone else from the kind of difficulty his grandmother endured, Peti is eager to try.