The results are in from a global-scale phase 3 clinical trial of the drug Eritoran, which doctors hoped would treat severe sepsis, and they are disappointing. According to Dr. Steven Opal, lead author of the study published March 20 in the Journal of the American Medical Association, the drug did not help patients at all compared to a placebo.
Eritoran had shown great promise in lab testing. It intervenes in the process by which chemicals called endotoxins, or LPS, which reside on gram-negative bacteria, trigger an overzealous immune response that ultimately shuts multiple organs down, leading to septic shock. Severe sepsis afflicts about 750,000 Americans every year and kills between and quarter and a half of them. This trial involved nearly 2,000 patients worldwide.
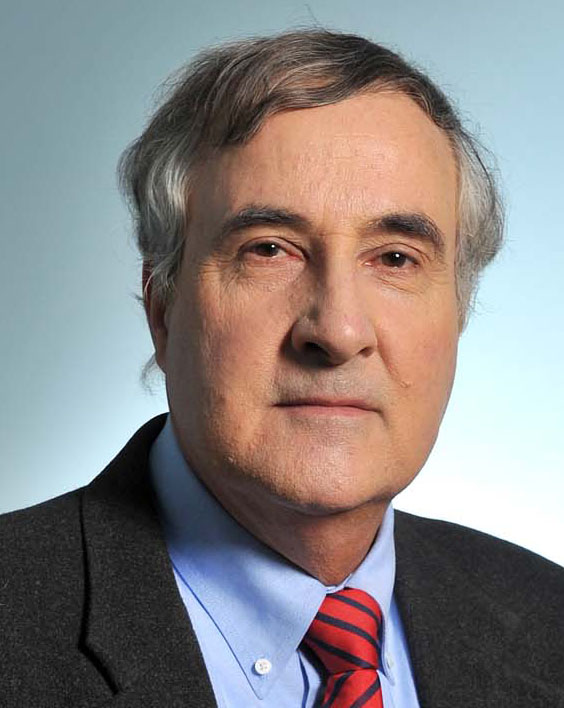
Opal, professor of medicine in the Warren Alpert Medical School of Brown University and an infectious disease physician at Memorial Hospital in Pawtucket, spoke with David Orenstein about the trial results and future research. The clinical research was funded by the drug maker Eisai Inc.
What is sepsis and what can doctors currently do about it?
It’s a major public health problem, which is largely unknown to the person on the street. It’s a very common cause of death worldwide. It’s typically a complication of other illnesses. A lot of people who have advanced cancer, or lots of other chronic debilitating illnesses, or are immunocompromised, actually wind up dying of septic shock. If you ask the families what happened to their loved one, they say he died of cancer, which is true, but the final event is often septic shock. But sometimes it occurs essentially out of the blue in healthy people and that makes it very dramatic. One example is toxic shock syndrome. People start off with a minor injury but then wind up with a necrotizing soft tissue infection and end up dying of toxic shock. We also see it in the hospitals among patients who come in with severe pneumonia.
It’s classically associated with an infection, but what distinguishes it from a localized infection is that the patient’s immune system, in trying to deal with this infection which is no longer that well localized, winds up being injurious to the body’s own physiology. It’s an innocent bystander kind of thing. If you have pneumonia, why are your kidneys failing? What’s happening is the host response has caused a systemic inflammatory response that contributes to the kidney’s injury.
What we do is what we’ve done for the last 35 years or so, which is disappointing. There really hasn’t been a lot of progress but there has been some. The treatment in a nutshell is to give patients intravenous fluids to re-establish their blood pressure. Give them antibiotics as soon as possible and give optimal supportive care, typically in the intensive care unit. If you look at the survival rate of people involved in septic shock in the 1980s versus the 2010s the mortality rate has gone down substantially. But it’s not because we do anything terribly different than what we’ve done all along. We just do it better and faster. There’s been an international effort to try to improve the outcome of septic shock called the Surviving Sepsis Campaign, and that has had a real effect. This really is a medical emergency.
What were the hopes for Eritoran that inspired the multinational phase 3 clinical trial?
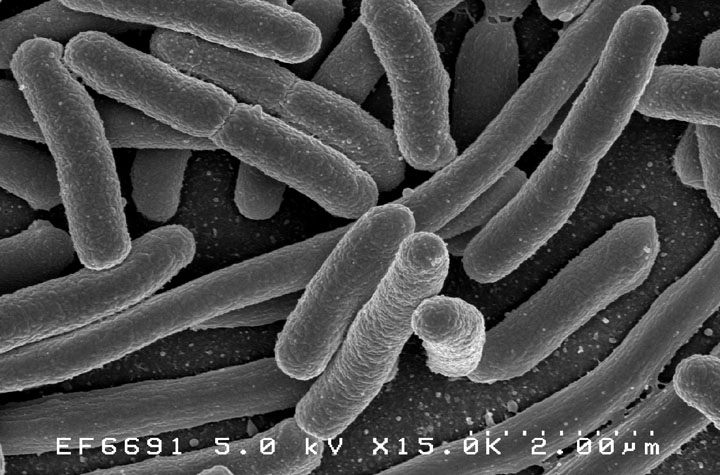
There’s been significant improvement and that’s great but what we haven’t seen is a major paradigm shift or some other new wonder drug that adds to the benefit, which is frustrating. A lot of things work in experimental models of sepsis. We can rescue animals much better with treatments, but in the clinic they haven’t worked. This drug, Eritoran, is very effective in mice. We were hoping it would work in humans, of course. The company that developed the drug spent a lot of time doing endotoxin challenges in normal human volunteers. The inhibitor would completely block it.
The real excitement of this treatment was that it was the first major international trial where the target was a relatively newly described receptor molecule known as the toll-like receptor. Bruce Beutler (et. al.) won the Nobel Prize in 2011 for the discovery of the toll-like receptors because it was the long-awaited recognition that there was a specific receptor on inflammatory cells that recognized endotoxin.
Another thing that made this experiment particularly interesting is that endotoxin was first recognized by Robert Koch and Richard Pfeiffer in the 1890s. It was evident that this is really important and if we had a treatment for it, it would be wonderful. People have been trying to come up with a strategy ever since.
Overall, what did you find?
The drug is very effective as an anti-endotoxin but it didn’t work if you give it to someone who is already infected and in established septic shock. That, of course was the hope, that we could still rescue people who were desperately ill, but we saw no signal whatsoever. It didn’t work, period. To me it answered the question, which has been around for over 100 years.
It’s either because it’s too late because the effect of endotoxin occurs within minutes and maybe that’s the critical time we’re missing, or perhaps more likely what happens is that after you get severely ill and you get a little bit of endotoxin into your circulation, you reprogram your cells to try to prevent dying from endotoxic shock. So the cell is reprogrammed for LPS tolerance to be less susceptible to the effects of endotoxin. This condition of LPS tolerance after even minute doses of endotoxin exposure has been known for decades in endotoxin research. By the time we clinically recognize what is going on, by the time we give the drug, the host cells may already be relatively refractory to endotoxin and it’s not going to work.
Does this close the door on any hope for the approach of blocking inflammatory response receptors, as Eritoran does?
A lot of other people who were thinking of developing other toll-like receptor inhibitors or other inhibitors for LPS were very disappointed with the initial results for the study because it suggested that maybe it’s not worth the effort.
I don’t see any reason to do any other trials with a TLR4 inhibitor like in this study. I think we proved pretty convincingly that it’s not going to work in established septic shock, at least as a single agent. However, there are 10 toll-like receptors in humans and it’s possible that if you added this inhibitor to inhibitors of others, it may still work. It’s not going to work as a single agent in established septic shock.
What else is in the pipeline now for sepsis?
There was a drug on the market for the last 10 years called activated protein C, which was the first and only drug that ever got approved for use specifically to treat septic shock. It was taken off the market a year and a half ago because in the second phase 3 trial they were unable to duplicate the results of the first phase 3 trial.
There are several things still in the pipeline. A large number of drugs for sepsis are in early stage development. One of the common treatments that have been tried for a long time is corticosteroids. They are still testing steroids in clinical trials. We still use them occasionally.
There’s another drug that we’re studying now called soluble thrombomodulin. It defends the microcirculation from injury during systemic inflammatory events and prevents intravascular clotting. Thrombomodulin is an endogenous protein found in capillaries. In sepsis the levels go way down. Replenishing this protein in animals works great in experimental sepsis models. We are now testing in human clinical trials.
There’s also another phase 3 trial using a hemoperfusion column where they take the blood of septic patients, pass it across a filtration column to absorb endotoxin, other microbial mediators, and host derived inflammatory mediators. The blood is then reperfused back into the patient. It’s a blood purification strategy. It’s the same sort of idea as hemodialysis.
There are still things being done, as septic shock is expected to increase in the future as the population ages. Sepsis is more common in the elderly. There is still plenty of room to improve the care and hopefully increase the survival rate from severe sepsis and septic shock.
I’m not the only doctor at Brown who studies sepsis. Mitchell Levy leads the Surviving Sepsis guidelines. Al Ayala in surgical research and a number of faculty members in pulmonary-critical care, surgery, and immunology work on basic and applied science in sepsis research.
