PROVIDENCE, R.I. [Brown University] — Nobody wins when patients stay in the hospital unnecessarily, so the federal government in recent years has pushed hospitals to be careful about admitting Medicare recipients as inpatients. The apparent result is that more patients are being “held for observation” instead, according to a new study by Brown University gerontologists. While the shift in how hospitals care for elderly patients in the emergency department may reduce costs to Medicare, it can also increase out-of-pocket expenditures for patients.
“The dual trends of increasing hospital observation services and declining inpatient admissions suggest that hospitals and physicians may be substituting observation services for inpatient admissions — perhaps to avoid unfavorable Medicare audits targeting hospital admissions,” the researchers wrote in their study published in the June edition of the journal Health Affairs.
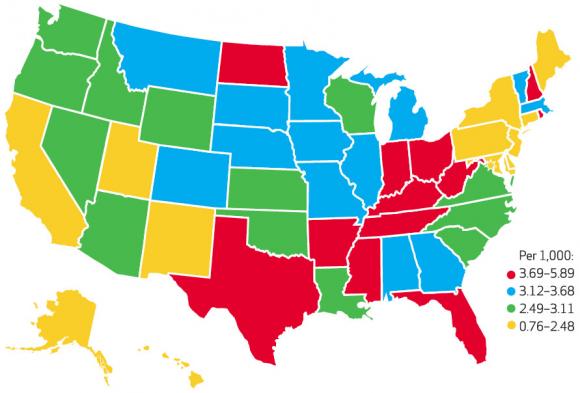
In the study, the researchers found that although the rate of observation stays varies widely by state and even by hospital, the nationwide ratio of Medicare patients who are “held for observation” to those who are admitted for inpatient stays increased 34 percent between 2007 and 2009.
Being held for observation, especially for days, can appear to patients to be exactly the same experience as being admitted — until they get the bill. That’s because people held for observation are classified as outpatients. Under Medicare rules, outpatients may face higher co-pays for their in-hospital services and won’t be covered for subsequent care in skilled nursing facilities. Zhanlian Feng, assistant professor of health services, policy, and practice and first author on the paper, said he first thought to conduct the study when he read media reports of patients who were surprised by their higher costs after spending nights in the hospital.
“They never thought they were being treated as outpatients,” Feng said.
More observation for longer
The practice has alarmed patient advocacy groups, one of which launched a class-action suit against the government last year. The groups had claimed the practice was increasing. Feng, a gerontology researcher in Brown’s Program in Public Health, figured he could contribute to the debate by determining whether that was true.
“I had not seen the numbers,” he said. “That really prompted me to do some real research.”
The results show that to a specific and significant degree, the increase is not just a perception. After reviewing Medicare records of 29 million fee-for-service Medicare beneficiaries 65 and older in 2007, 2008, and 2009, Feng and his two co-authors found several trends:
- Observation stays rose to 1,019,881 (involving 2.9 per 1,000 beneficiaries) in 2009 from 814,692 (2.3 per 1,000 beneficiaries) in 2007;
- Inpatient admissions fell to 22.5 per 1,000 beneficiaries in 2009 from 23.9 per 1,000 in 2007;
- Observation stays got an average of 7 percent longer over the study period;
- In 2009, 44,843 patients were held for observation longer than 72 hours, compared to 23,841 in 2007;
- By state, observation stay rates in 2009 varied from a low of 0.8 per 1,000 beneficiaries in New York to 5.9 per 1,000 in West Virginia.;
Federal pressure
In its efforts to contain Medicare costs by preventing unnecessary hospitalization, the government has pulled several new levers in the last decade. In 2006 officials signaled an increase in audits of inpatient admissions, and in 2004 they allowed hospitals to change a patient’s status retroactively from inpatient to outpatient with observation before discharge. Most recently, the Affordable Care Act of 2010 includes a provision penalizing hospitals if they have high readmission rates. Classifying patients as outpatients, either on their first or second visit, helps hospitals steer clear of counting them as readmitted.
Feng said he hopes the research will help policymakers better understand the facts surrounding the controversial issue. One area for further investigation, he said, could be to determine the clinical circumstances that led tens of thousands of patients to be held for observation for longer than three days. Another could be to determine how many patients held for observation actually faced any financial consequences for holding the outpatient versus inpatient designation.
In addition to Feng, the paper’s other authors were Vincent Mor, professor of health services, policy, and practice, and postdoctoral research fellow Brad Wright.
Funding for the research came from the Retirement Research Foundation (Grant 2011-066) and the National Institute on Aging (Grant P01AG027296).