PROVIDENCE, R.I. [Brown University] — On April 12, 2011, nearly 15 years after she became paralyzed and unable to speak, a woman controlled a robotic arm by thinking about moving her arm and hand to lift a bottle of coffee to her mouth and take a drink. That achievement is one of the advances in brain-computer interfaces, restorative neurotechnology, and assistive robot technology described in the May 17 edition of the journal Nature by the BrainGate2 collaboration of researchers at the Department of Veterans Affairs, Brown University, Massachusetts General Hospital, Harvard Medical School, and the German Aerospace Center (DLR).
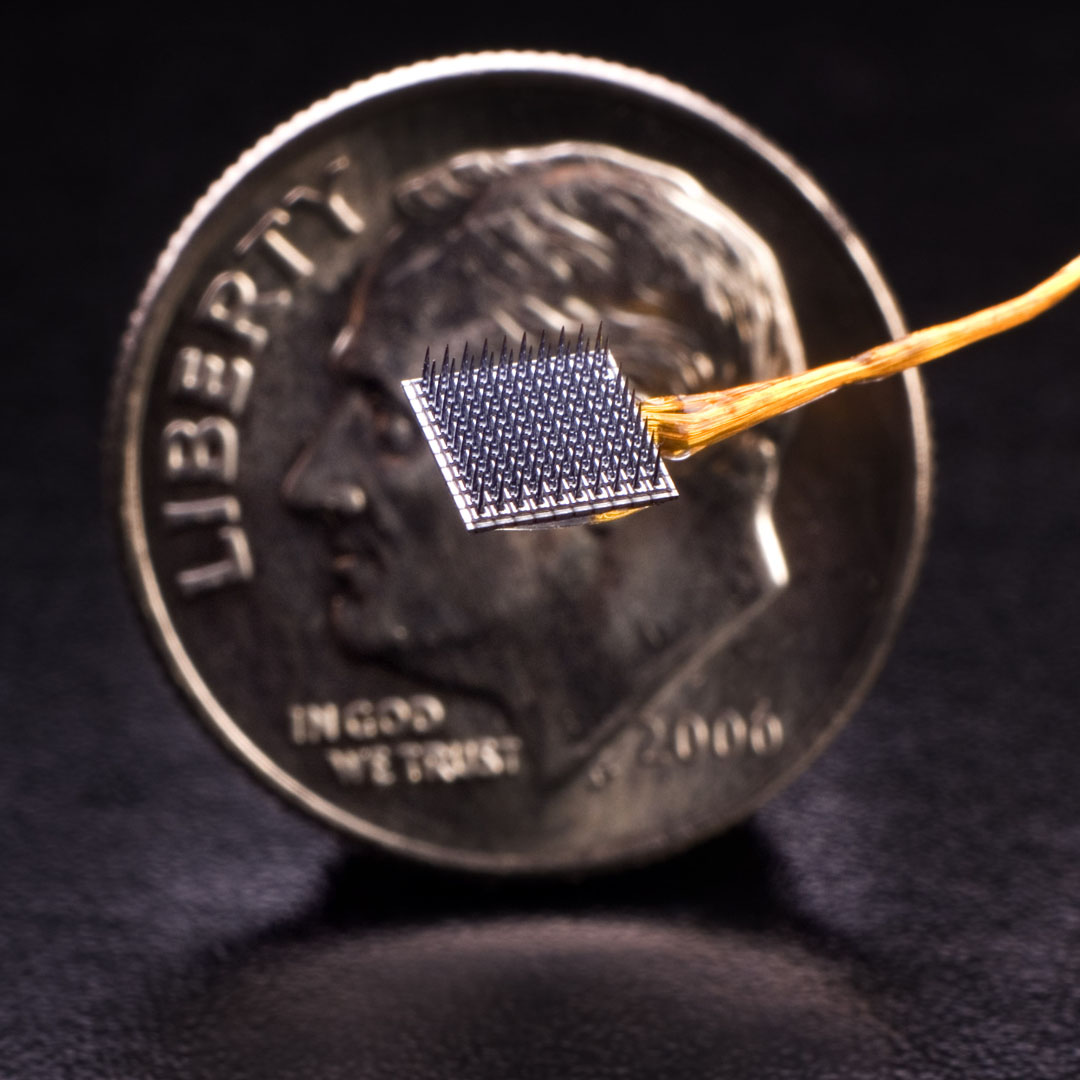
A 58-year-old woman (“S3”) and a 66-year-old man (“T2”) participated in the study. They had each been paralyzed by a brainstem stroke years earlier which left them with no functional control of their limbs. In the research, the participants used neural activity to directly control two different robotic arms, one developed by the DLR Institute of Robotics and Mechatronics and the other by DEKA Research and Development Corp., to perform reaching and grasping tasks across a broad three-dimensional space. The BrainGate2 pilot clinical trial employs the investigational BrainGate system initially developed at Brown University, in which a baby aspirin-sized device with a grid of 96 tiny electrodes is implanted in the motor cortex — a part of the brain that is involved in voluntary movement. The electrodes are close enough to individual neurons to record the neural activity associated with intended movement. An external computer translates the pattern of impulses across a population of neurons into commands to operate assistive devices, such as the DLR and DEKA robot arms used in the study now reported in Nature.
BrainGate participants have previously demonstrated neurally based two-dimensional point-and-click control of a cursor on a computer screen and rudimentary control of simple robotic devices.
The study represents the first demonstration and the first peer-reviewed report of people with tetraplegia using brain signals to control a robotic arm in three-dimensional space to complete a task usually performed by their arm. Specifically, S3 and T2 controlled the arms to reach for and grasp foam targets that were placed in front of them using flexible supports. In addition, S3 used the DLR robot to pick up a bottle of coffee, bring it to her mouth, issue a command to tip it, drink through a straw, and return the bottle to the table. Her BrainGate-enabled, robotic-arm control during the drinking task required a combination of two-dimensional movements across a table top plus a “grasp” command to either grasp and lift or tilt the robotic hand.
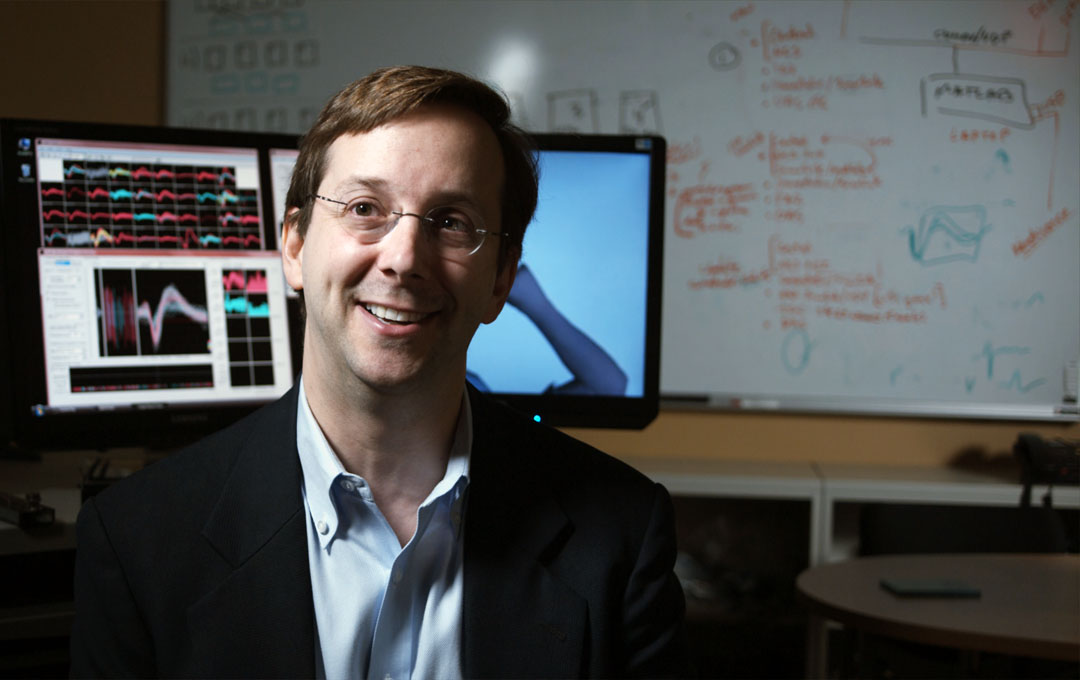
“Our goal in this research is to develop technology that will restore independence and mobility for people with paralysis or limb loss,” said lead author Dr. Leigh Hochberg, a neuroengineer and critical care neurologist who holds appointments at the Department of Veterans Affairs, Brown University, Massachusetts General Hospital, and Harvard. He is the sponsor-investigator for the BrainGate2 pilot clinical trial. “We have much more work to do, but the encouraging progress of this research is demonstrated not only in the reach-and-grasp data, but even more so in S3’s smile when she served herself coffee of her own volition for the first time in almost 15 years.”
Partial funding for this work comes from the VA, which is committed to improving the lives of injured veterans. “VA is honored to have played a role in this exciting and promising area of research,” said VA Secretary Eric Shinseki. “Today’s announcement represents a great step forward toward improving the quality of life for veterans and others who have either lost limbs or are paralyzed.”
Hochberg adds that even after nearly 15 years, a part of the brain essentially “disconnected” from its original target by a brainstem stroke was still able to direct the complex, multidimensional movement of an external arm — in this case, a robotic limb. The researchers also noted that S3 was able to perform the tasks more than five years after the investigational BrainGate electrode array was implanted. This sets a new benchmark for how long implanted brain-computer interface electrodes have remained viable and provided useful command signals.
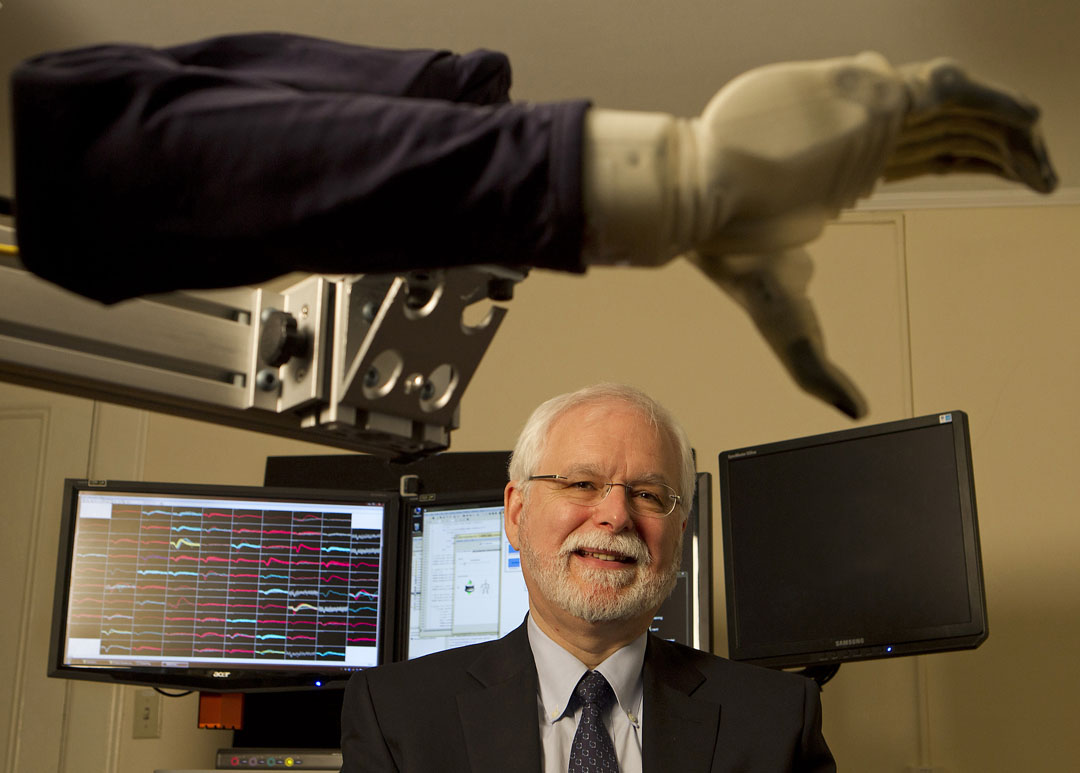
John Donoghue, the VA and Brown neuroscientist who pioneered BrainGate more than a decade ago and who is co-senior author of the study, said the paper shows how far the field of brain-computer interfaces has come since the first demonstrations of computer control with BrainGate.
“This paper reports an important advance by rigorously demonstrating in more than one participant that precise three-dimensional neural control of robot arms is not only possible, but also repeatable,” said Donoghue, who directs the Brown Institute for Brain Science. “We’ve moved significantly closer to returning everyday functions, like serving yourself a sip of coffee, usually performed effortlessly by the arm and hand, for people who are unable to move their own limbs. We are also encouraged to see useful control more than five years after implant of the BrainGate array in one of our participants. This work is a critical step toward realizing the long-term goal of creating a neurotechnology that will restore movement, control, and independence to people with paralysis or limb loss.”
In the research, the robots acted as a substitute for each participant’s paralyzed arm. The robotic arms responded to the participants’ intent to move as they imagined reaching for each foam target. The robot hand grasped the target when the participants imagined a hand squeeze. Because the diameter of the targets was more than half the width of the robot hand openings, the task required the participants to exert precise control. (Videos of these actions are available on the Nature website.)
In 158 trials over four days, S3 was able to touch the target within an allotted time in 48.8 percent of the cases using the DLR robotic arm and hand and 69.2 percent of the cases with the DEKA arm and hand, which has the wider grasp. In 45 trials using the DEKA arm, T2 touched the target 95.6 percent of the time. Of the successful touches, S3 grasped the target 43.6 percent of the time with the DLR arm and 66.7 percent of the time with the DEKA arm. T2’s grasp succeeded 62.2 percent of the time.
T2 performed the session in this study on his fourth day of interacting with the arm; the prior three sessions were focused on system development. Using his eyes to indicate each letter, he later described his control of the arm: “I just imagined moving my own arm and the [DEKA] arm moved where I wanted it to go.”
The study used two advanced robotic arms: the DLR Light-Weight Robot III with DLR five-fingered hand and the DEKA Arm System. The DLR LWR-III, which is designed to assist in recreating actions like the human arm and hand and to interact with human users, could be valuable as an assistive robotic device for people with various disabilities. Patrick van der Smagt, head of bionics and assistive robotics at DLR, director of biomimetic robotics and machine learning labs at DLR and the Technische Universität München, and a co-senior author on the paper said: “This is what we were hoping for with this arm. We wanted to create an arm that could be used intuitively by varying forms of control. The arm is already in use by numerous research labs around the world who use its unique interaction and safety capabilities. This is a compelling demonstration of the potential utility of the arm by a person with paralysis.”
DEKA Research and Development developed the DEKA Arm System for amputees, through funding from the United States Defense Advanced Research Projects Agency (DARPA). Dean Kamen, founder of DEKA said, “One of our dreams for the Luke Arm [as the DEKA Arm System is known informally] since its inception has been to provide a limb that could be operated not only by external sensors, but also by more directly thought-driven control. We’re pleased about these results and for the continued research being done by the group at the VA, Brown and MGH.” The research is aimed at learning how the DEKA arm might be controlled directly from the brain, potentially allowing amputees to more naturally control this prosthetic limb.
Over the last two years, VA has been conducting an optimization study of the DEKA prosthetic arm at several sites, with the cooperation of veterans and active duty service members who have lost an arm. Feedback from the study is helping DEKA engineers to refine the artificial arm’s design and function. “Brain-computer interfaces, such as BrainGate, have the potential to provide an unprecedented level of functional control over prosthetic arms of the future,” said Joel Kupersmith, M.D., VA chief research and development officer. “This innovation is an example of federal collaboration at its finest.”
Story Landis, director of the National Institute of Neurological Disorders and Stroke, which funded the work in part, noted: “This technology was made possible by decades of investment and research into how the brain controls movement. It’s been thrilling to see the technology evolve from studies of basic neurophysiology and move into clinical trials, where it is showing significant promise for people with brain injuries and disorders.”
In addition to Hochberg, Donoghue, and van der Smagt, other authors on the paper are Daniel Bacher, Beata Jarosiewicz, Nicolas Masse, John Simeral, Joern Vogel, Sami Haddadin, Jie Liu, and Sydney Cash.
Additional comments
Vincent Ng
Medical Center Director, Providence VA Medical Center
“The VA is on the forefront of translational research that’s improving the quality of life for our Veterans who have sacrificed so much for our Nation. We are proud to be a part of this exciting, collaborative research.”
U.S. Sen. Sheldon Whitehouse
“I congratulate Brown University and the Providence VA Medical Center for this ground-breaking project, which could help to significantly improve the quality of life of disabled and paralyzed Americans, including many veterans. The innovations produced in this new study highlight the value of federal support for basic scientific research.”
U.S. Rep. David Cicilline
“I congratulate the entire Brown University community on the progress it has made in this project. It is my hope that with continued success, this advancement will help improve the quality of life for individuals with disabilities, especially our men and women in uniform.”
Jennifer French
Executive Director, Neurotech Network
“This latest development in cortical control research has the potential to revolutionize the way we interact with technology. More specifically, the possibilities open a new level of independence for those living with severe paralysis. Simple tasks like drinking, eating or brushing your teeth are not possible for people living with severe paralysis. The ability to perform these every-day tasks can create a new world of independence for people with severe disabilities.”
R. John Davenport
Associate Director, Brown University Institute for Brain Science
“This exciting advance from the BrainGate team exemplifies the amazing science that can only result when researchers from disparate disciplines collaborate. The Institute works to link fundamental science, engineering, and medicine among our more than 100 faculty members.”
The BrainGate2 study continues to enroll participants to take part in this research and recently added Stanford University as a member of the collaboration and a clinical trial site.
About the BrainGate collaboration
This advance is the result of the ongoing collaborative BrainGate research at Brown University, Massachusetts General Hospital, Providence VA Medical Center; researchers at Stanford University have recently joined the collaboration as well. The BrainGate research team is focused on developing and testing neuroscientifically inspired technologies to improve the communication, mobility, and independence of people with neurologic disorders, injury, or limb loss.
Funding for the study and its projects comes from the Rehabilitation Research and Development Service, Office of Research and Development, U.S. Department of Veterans Affairs, the National Institutes of Health (some grants were funded all or in part through the American Recovery and Reinvestment Act), the Eunice Kennedy Shriver National Institute of Child Health and Human Development/National Center for Medical Rehabilitation Research (HD53403, HD100018, HD063931), the National Institute on Deafness and Other Communication Disorders, the National Institute of Neurological Disorders and Stroke (NS025074), the National Institute of Biomedical Imaging and Bioengineering (EB007401), the Doris Duke Charitable Foundation, the MGH-Deane Institute for Integrated Research on Atrial Fibrillation and Stroke, Katie Samson Foundation, and the Craig H. Neilsen Foundation. The contents do not represent the official views of the Department of Veterans Affairs or the United States Government.
The implanted microelectrode array and associated neural recording hardware used in the BrainGate research are manufactured by BlackRock Microsystems LLC (Salt Lake City, Utah). The research prototype Gen2 DEKAarm was provided by DEKA Integrated Solutions Inc, under contract from the Defense Advanced Research Project Agency (DARPA).
The BrainGate pilot clinical trial was previously directed by Cyberkinetics Neurotechnology Systems Inc. Foxborough, Mass., (CKI). CKI ceased operations in 2009, before the collection of data reported in the Nature manuscript. The clinical trials of the BrainGate2 Neural Interface System are now administered by Massachusetts General Hospital, Boston, Mass. Donoghue is a former chief scientific officer and a former director of CKI; he held stocks and received compensation. Hochberg received research support from Massachusetts General and Spaulding Rehabilitation Hospitals, which in turn received clinical trial support from Cyberkinetics.
CAUTION: Investigational Device. Limited by Federal Law to Investigational Use. The device is being studied under an IDE for the detection and transmission of neural signals from the cortex to externally powered communication systems, environmental control systems, and assistive devices by persons unable to use their hands due to physical impairment. The clinical trial is ongoing; results presented are thus preliminary. The safety and effectiveness of the device have not been established.
Press contacts
David Orenstein, Brown University, [email protected], 401-527-2525
Mark Ballesteros, U.S. Dept. of Veterans Affairs, [email protected], 202-461-7559.
Michael Morrison, Massachusetts General Hospital, [email protected], 617-724-6425

