PROVIDENCE, R.I. [Brown University] — In the last decade, minorities have poured into nursing homes at a time when whites have left in even greater numbers, according to a new Brown University study that suggests a racial disparity in elder care options in the United States.
At first blush the analysis, published July 7 in the journal Health Affairs, suggests that elderly blacks, Hispanics, and Asians are gaining greater access to nursing home care. But the growing proportion of minorities in nursing homes is coming about partly because they do not have the same access to more desirable forms of care as wealthier whites do, said the study’s lead author Zhanlian Feng, assistant professor of community health in the Warren Alpert Medical School of Brown University.

Credit: David Orenstein/Brown University
“Seemingly, we are closing the gap in terms of minority access to nursing home beds, but I don’t think that is something to celebrate,” Feng said. “They are really the last resort. Most elders would rather stay in their homes, or some place like home, but not a nursing home unless they have to.”
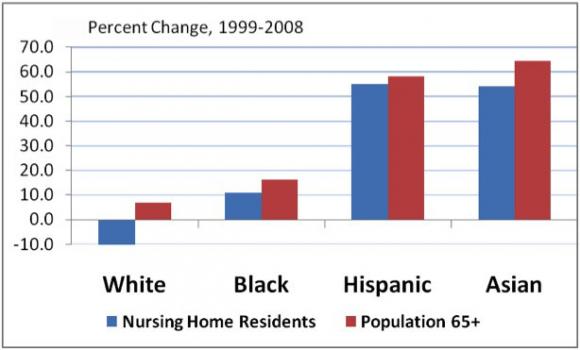
The new analysis shows that between 1999 and 2008 the nation’s nursing home population shrank by 6.1 percent to just over 1.2 million people. In that time period the number of whites in nursing homes decreased by 10.2 percent nationwide, while the number of blacks rose 10.8 percent, the number of Hispanics rose by 54.9 percent and the number of Asians rose by 54.1 percent. The study also looked at nursing home population changes in the top 10 metropolitan areas for each minority.
Prior research has shown that the nursing homes in predominately minority areas are often of lower quality and are more likely to close, while assisted living facilities are more likely to be built in areas where residents have high incomes. The result, reflected in the figures in the new Health Affairs paper, is a disparity that plays out not only economically and geographically, but also racially, Feng said.
“We know those alternatives are not equally available, accessible, or affordable to everybody, certainly not to many minority elders,” he said.
As policymakers look to “rebalance” elder care from nursing homes to other forms of care, for instance with shifts in Medicaid funding to support home and community-based services, they should account for these disparities, Feng said. As it is, whites are clearly more likely to be using more desirable alternatives; more concerted efforts may be required to promote minority elders’ use of them too, he said.
“Rebalancing is a recognition of most people’s preferences for long-term care,” Feng said. “For that effort to be successful you have to consider who is using what.”
To determine the figures, Feng and his co-authors used the federally mandated Minimum Data Set, which tracks the population of nursing home users and assesses their care needs on a routine basis, because they receive substantial Medicare and Medicaid funding. Similar data is not available for other kinds of elder care, which is predominantly paid for with private insurance dollars.
Metropolitan shifts
One way Feng and his co-authors have quantified the disparity in eldercare is by grouping metropolitan areas into quartiles based on the proportion of whites, blacks, Hispanics or Asians 65 or older in each area. The researchers found that the representation of blacks, Hispanics and Asians in nursing homes increased as their share of elderly in the total population increased. That correlation did not hold for whites, who did not appear to be obliged to choose nursing homes as they age.
In New York, a top 10 metropolitan area for blacks, Hispanics and Asians, nursing home residents from these groups increased 22 percent, 84 percent and 40 percent, respectively. In Los Angeles/Long Beach, the increases were 1 percent for blacks, 41 percent for Hispanics and 56 percent among Asians.
With different rates in different cities, the challenge facing policymakers is not only national, but also local, the researchers said.
“Efforts to reduce disparities should target both communities and facilities with high concentrations of minority residents,” they wrote in Health Affairs.
In addition to Feng, the paper’s other authors at Brown are Mary Fennell, professor of sociology; Denise Tyler, gerontology researcher; Melissa Clark, associate professor of community health; and Vincent Mor, the Florence Pirce Grant Professor of Health Services, Policy, and Practice.
The National Institute on Aging supported the research.