PROVIDENCE, R.I. [Brown University] — The rate at which lead poisoning has struck young Rhode Island children depends heavily on where they live, according to a Brown University-led geographic analysis of comprehensive health department data from across Rhode Island between 1993 and 2005. By mapping cases of lead poisoning, researchers have been able to help target cleanup resources to do the most good.
During that 12-year period, some census blocks in the state had no cases of poisoning in the study group of 204,746 children, but in the hardest hit census blocks of Providence, Pawtucket, Central Falls, Woonsocket, and Newport, lead poisoning afflicted as many as 48.6 percent of kids under 6.
Patrick Vivier, associate professor of community health and pediatrics and lead author of the study, said that although he has been familiar with the state’s fight against lead poisoning for years, he was still struck by the geographic and demographic disparities uncovered in the analysis published online Oct. 23 by Maternal and Child Health Journal.
“We know there are disparities, but to look at zero cases in some areas and almost 50 percent in some areas is still shocking,” said Vivier, who is also affiliated with Hasbro Children’s Hospital and Rhode Island Hospital.

Although the trend over time has been that lead poisoning cases are declining, that does not mean the problem’s impact has dissipated. The damage lead can do to a child’s developing nervous system is irreversible. In hard-hit areas, a generation of children has been at high risk for suffering symptoms such as behavioral disorders and reduced attention span and IQ scores.
Pinpointing poisoning
According to the study of state health department mandated test results, the risk of a child being poisoned by lead was four times higher than average for children living in the state’s poorest neighborhoods, and just under three times higher for children living in a neighborhood with a preponderance of pre-1950 housing. Sometimes those areas overlapped, but even accounting for that overlap, each factor independently and significantly heightened the risk kids faced.
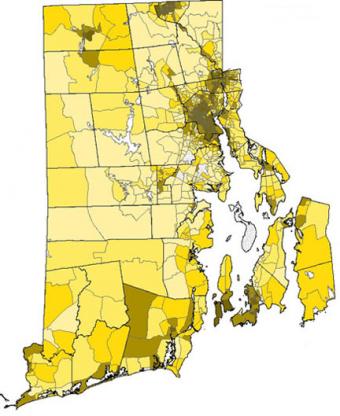
Viewed on maps, the data make a clear case that lead poisoning is a much greater problem in some very specific areas of the state than in others, Vivier said. This insight has allowed a commission formed by Attorney General Patrick Lynch to recommend the best places to spend millions of dollars of cleanup money provided by DuPont after years of protracted litigation by the attorney general against several chemical companies and paint manufacturers.
The commission used the data to map the neighborhoods that had the highest poverty, the highest stock of pre-1950 housing and the highest frequency of lead poisoning, and focused the efforts there.
“We know where to go,” Vivier said. “These places are clustered in specific spots so it means we can go and do something about it in those places.”
Cleanup efforts around the state funded by the Du Pont money are still going on.
Rhode Island’s mandatory program of testing for lead poisoning and the Rhode Island Department of Health’s statewide lead database have provided an unusually rich record of data, Vivier said. But looking at the striking sociological disparities in the data, as well as its usefulness in mapping those disparities, Vivier said public health researchers should be eager to apply geographic analysis in other such studies.
“This paper demonstrates the huge health burden that where you live can have,” Vivier said.
In addition to Vivier, the study’s other authors were Sherry Weitzen, research assistant professor of community health; John Logan, professor of sociology; Marissa Hauptman of New York University Medical School; Scott Bell, associate professor of geography at the University of Saskatchewan; and Daniela Quilliam of the Rhode Island Department of Health.
The study was funded by Brown University, including money received from Du Pont as part of an agreement between the company and state Attorney General Patrick Lynch.