PROVIDENCE, R.I. [Brown University] — Contrary to conventional wisdom, scientific evidence proving that overlapping multiple sexual partners — concurrency — drives the HIV epidemic in sub-Saharan Africa is actually quite limited, Brown University researchers have concluded.
As a result, they say, far more research is needed to prove what has been a long-held assertion for close to 15 years — that the sexual practice of concurrency has accelerated the spread of HIV in Africa.
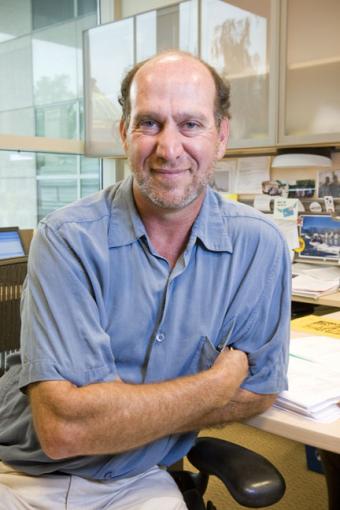
“People have just accepted at face value that this is the main thing that’s driving the epidemic,” said epidemiologist Mark Lurie, assistant professor community health and medicine. “But the evidence that concurrency is a major factor is very weak.”
Lurie and co-author Samantha Rosenthal detail their argument in an upcoming issue of the journal AIDS and Behavior. The article is available online now. Rosenthal is a graduate student in public health at Brown.
Lurie and Rosenthal say there is no conclusive evidence that overlapping multiple sexual partners increases the size of an HIV epidemic, accelerates the speed at which the virus is transmitted or makes HIV more persistent in a given population. They drew their conclusion by looking at previous studies that examined concurrency in any way.
The reason, they say, is that HIV epidemics can’t be explained by a single variable. A number of factors are more likely, with some factors more important in some geographic areas than others.
“The studies you need to prove causality don’t exist,” Lurie said. “None of those studies have been done.”
The researchers don’t dispute the notion that concurrent sexual relationships could “theoretically” play a major role driving HIV transmission through networks of people. But before this can be proven true, Lurie and Rosenthal say, a number of research initiatives are needed including:
- improved methods for measuring both sexual behavior and the duration or overlapping of sexual partnerships;
- a common definition of concurrency. Lurie and Rosenthal write that concurrency is defined many different ways in health literature, which complicates scientific measurement of its affects on HIV transmission. Some measurements, for example, only count ongoing sexual relationships and not casual partnerships;
- longitudinal studies that measure both concurrency and incidence of HIV infection. This is needed, the researchers said, to accurately determine whether there is a link between concurrent sexual relationships and increased HIV transmission.
Without the added data, Lurie said, there is a risk that public policy-makers, development agencies, and aid organizations are spending too much money on campaigns against taking on overlapping multiple sexual partners when other causes may matter more.
“We are also worried about the unintended consequences of concurrency interventions,” Lurie said. “If you are giving a message that says ‘Don’t have concurrent partnerships,’ then people can easily take away from that the message to have lots of partnerships as long as they don’t overlap.”
The result, Lurie said, leads to a waste of resources and “considerable harm” to a population that could inadvertently end up spreading HIV.
Lurie and Rosenthal said the paper has already drawn interest from officials at the World Health Organization, the Centers for Disease Control and Prevention, and other organizations. They have also been invited to speak about their work at the University of Cape Town and Columbia University School of Public Health.
A grant from the National Institute of Mental Health, given through the National Institutes of Health, helped fund the study.